
Positron Emission Tomography (PET) is combined with CT to provide unique non-invasive, sensitive, accurate and functional imaging of the body. Depending on the type of radioactive material used, various types of conditions can be imaged accordingly. The most commonly radioactive material used worldwide is 18F-FDG, which is a glucose-analog that enables clinicians to map the metabolic activities within the body. Cells which have higher metabolic activities such as cancer would have higher 18F-FDG uptake; thus appearing hotter (highlighted) in the scan. The procedure is very safe and radiation exposure from the scan is relatively low.


Single Photon Emission Computed Tomography (SPECT-CT) is a hybrid imaging similar to PET-CT; providing sensitive, precise and targeted imaging on how different parts of the body are working. The fundamental differences between the two hybrid imaging are the types of radioactive materials used, where SPECT-CT is able to perform a wider range of radioactive imaging. Similarly, the procedure is very safe and radiation exposure from the scan is relatively low.



Radioiodine-131 therapy is a type of nuclear medicine therapy which uses radioactive iodine(I-131) to destroy thyroid cells. This therapy is used to treat hyperthyroidism and thyroid cancer.
Hyperthyroidism occurs when the thyroid gland produces excessive hormones either due to hyper-functioning nodule(s) or the whole gland per se. Radioiodine-131 would target and destroy these hyperfunctioning thyroid cells and sparing “normal” thyroid cells; restoring the normal functions of the thyroid gland.
In thyroid cancer, radioiodine-131 therapy is usually performed following surgical removal of the thyroid glands. Radioiodine-131 would basically destroy any remnant or metastatic thyroid tissue. Though the name itself may seem terrifying, radioiodine-131 is a rather simple treatment where the radioactive is administered orally only once per course of treatment. As it is a targeted therapy, the side effects are minimal with the low risk of secondary cancers.
The treatment is very effective and is safely administrated under supervision of Nuclear Medicine Physician.
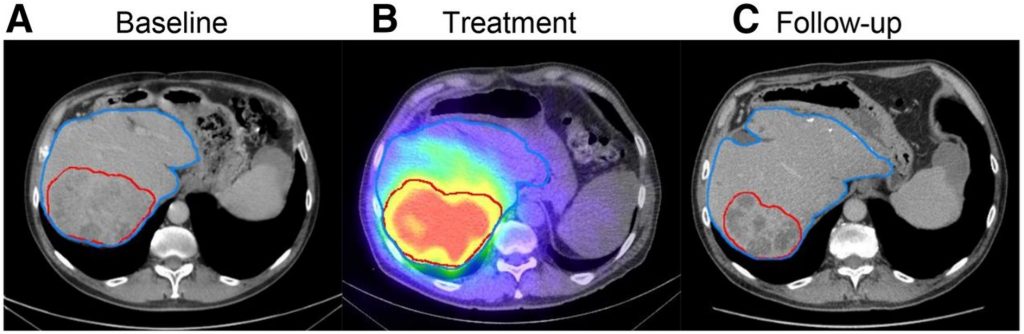
Selective Internal Radiation Therapy (SIRT) is used for the treatment of patients with hepatocellular cancer and colorectal liver metastases. In this therapy, Yyttrium-90 microspheres are embolised into the hepatic artery supplying the tumors. Lethal doses of radiation can be delivered safely to tumours while ensuring that the dose received by the non-tumorous areas of liver is within the tolerable levels (avoiding development of serious or even fatal radiation hepatitis).
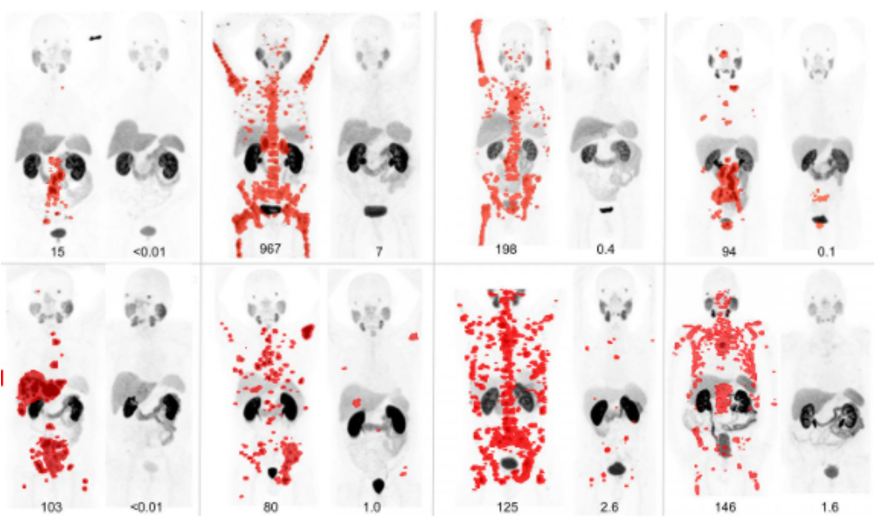
Lutetium-177 PSMA (Prostate specific membrane antigen) treatment is a form of nuclear medicine therapy that targets and destroys prostate cancer cells that have spread into parts of the body, including lymph nodes and bones. The destruction of the metastatic prostate cancer cells has been shown to prolong life expectancy and alleviate any metastatic-related symptoms such as bone pain.
Radiosynovectomy is used to treat painful joints caused by synovitis. This rather simple therapy destroys the synovial tissue that causes joint swelling without causing much harm to the rest of the body due to the unique property of the radioactive which only travel a short distance (average maximum range of 3.6 mm). The injection of the radioactive into the joint destroy abnormal synovial and thus reducing joint inflammation and deformity.
Bone metastasis is a major complication of several solid cancers such as prostate and breast, cancers. For solitary metastasis, surgery or radiation therapy would be usually performed but for extensive bone metastases, systemic treatment would be needed. In most cases of extensive bone metastases, bone pain is an issue. Therefore, radiopharmaceuticals such as strontium-89, radium-223 and samarium-153 can be used for the treatment of bone metastases; providing targeted therapy with minimal side effects and improvement in quality of life.
Monday - Thursday: 8:30am - 5:00pm
Friday: 8:30am - 4:30pm
Saturday & Sunday: Closed
Malaysia Website Design, Lightflex.